Luteal phase support in ART - ppt video online download
4.8 (403) In stock
4.8 (403) In stock
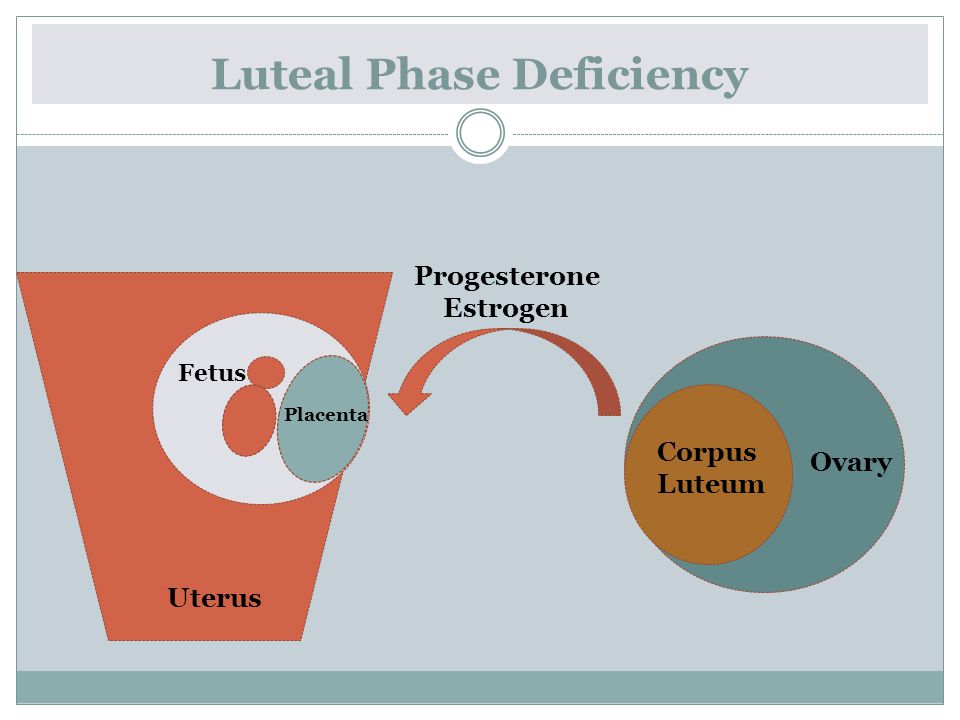
The cause of the Luteal phase defect in stimulated IVF cycles Debatable for more than tow decades Removal of large quantities of granulose cells during the OR might diminish an important sources of progesterone syntheses This was not proven in natural cycles. Another theory that prolonged suppression by GnRH agonist will lead to suppression of LH production wich is important for support of corpuses Luteum HCG will also suppress production via short loop feed back mechnism. However, administration of HCG did not suppress the LH secretion in an stimulated cycle.
Luteal phase support in ART
By DR. Zeinab Abotalib MRCOG Consultant & Associate Prof. Infertility & IVF.
Debatable for more than tow decades. Removal of large quantities of granulose cells during the OR might diminish an important sources of progesterone syntheses. This was not proven in natural cycles. Another theory that prolonged suppression by GnRH agonist will lead to suppression of LH production wich is important for support of corpuses Luteum. HCG will also suppress production via short loop feed back mechnism. However, administration of HCG did not suppress the LH secretion in an stimulated cycle.
The introduction of GnRH antagonist in IVF may obviate the need for LPS. This could not be evaluated because of premature luteolysis in IVF cycles which lead to unacceptable low pregnancy rate.
LPS has consisted of HCG; P; P plus HCG, E, ascorbic acid, aspirin or prednisolone. Different combinations, doses, durations & formulations are used, but the best dose, duration or formulation of treatment remains controversial.
To review RCTs & meta-analyses concerning LPS in ART. Materials & methods. An electronic search of the Cochrane library, Pub Med for RCT & meta-analyses concerning LPS from 1990 to
no Cochrane systematic review were found. Studies were classified into long, short, ultra-short & direct protocol studies.
P support was reviewed as regard the type, dose, route of administration, when to start & when to stop.
I. Luteal phase support in long protocol
Progesterone Vs no treatment: a significantly higher PR in groups treated with IM or oral P compared with no treatment (8 RCTs,Soliman et al, 1994) A. Progesterone.
IM Vs oral: IM P conferred the most benefit compared with oral P (meta-analysis, Prittis & Atwood, 2002) IM P (50 mg/day) resulted in significantly higher IR, CPR compared with oral P (600 mg/day) (Casini et al,2003). 4/30 women discontinued treatment because of their inability to administer IM P.
Vaginal P is as effective as the IM P & is associated with fewer side effects & greater patient adherence & satisfaction (10 RCT,Felicia et al ,2003). Adequate tissue levels of P after vaginal P is attributed to uterine first-pass effect.
The C & OPR were significantly lower with the oral formulation (Pouly et al, 1996; Frieder et al, 1999, Sucedo et al, 2000). These studies strongly suggest the inferiority of oral P for LPS. 1. The vaginal administration of P results in a greater bioavailability with less relative variability than oral P (Levine & Watson, 2000). 2. Oral P is subjected to first-pass pre-hepatic & hepatic metabolism.
2. IM: 25 mg IM P was compared with 100 mg P. No difference in CPR (Check et al,1991)..
1. Vaginal: Pezino et al (2004) compared. Gel (Crinone 8%, 90 mg/day), Capsules (Uterogestan 200 mg twice daily) & Suppositories (cyclogest 200 mg daily). No differences in CPR. Cost & minor side effects (perineal irritation, leaking out, interference with coitus) may limit the gel in favor of capsules & suppositories.
2. IM: 50 mg/d of IM P Vs 341 mg. /3 days (Costabile et al,2001) or. once weekly (Abte et al,1997) of IM 17 OH progesterone caproate. No differences in CPR or OPR.
Day of OR Vs day of ET: No difference (Baruffi et al,2002).
At 8 W (Costabile et al, 2001) At W (Check et al, 1991).
Most treatment protocols advocate the use of P throughout the first trimester, based on the findings of Shamma et al, who used 17-OH P as a marker to demonstrate ongoing corpus luteum activity up to week 10 of pregnancy.
LPS beyond the pregnancy test may not be indicated (Penzias,2002; Jacobs & Balen,2003).
The assumption that high serum P levels are required to achieve biological efficacy in the endometrium appears to be incorrect (Penzias,2000)
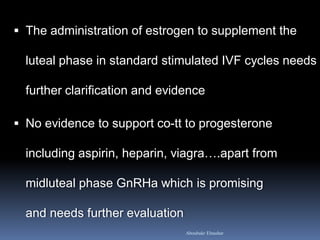
The oral estrogen doses: 2 to 6 mg /d. 1. No advantage. (Lewin et al, 1994; Smitz et al,1993;Tay & Lenton, 2003; Rashidi et al,2004).
3. Beneficial effect on PR in patients with profound E2 decline (E2 on day of HCG/ E2 of ET >50%) (Lakkis et al,2002; Gleicher et al,2000).
5000 IU/3d: no statistically significant differences in CPR (Ludwig et al,2001) IU midluteal. No affect on PR, but it helps to preserve corpus luteum function & avoids the need for further supplementation during early pregnancy (Herman et al,1996)
No benefit (Griesinger et al, 2002)
Prednisolone (15 mg daily following ET) does not improve the clinical pregnancy or implantation rates (Ezzeldin et al, 2003). The sample size of this study was small.
No benefit on PR , but it may reduce the rate of spontaneous pregnancy loss (Mollo et al,2003)
A significantly higher PR (Meta-analysis of 5 RCTs, Soliman et al, 1994) Many clinics have now stopped giving HCG because OHSS is not always easy to predict (Jacobs &Balen,2003). B. HCG.
CPR & OPR were not different (Albert & Pfeifer, 1991, Claman et al,1992; Araujo et al,1994; Artini et al,1995; Loh & Leong,1996; Claman et al,1992; Artni et al,1995).
3. HCG Vs vaginal P: No differences in CPR, OPR or SAB. (Artini et al,1995; Martinez et al,2000; Ludwig et al,2001; Ugur et al,2001).
5. HCG Vs IM P plus oestrogen: There were no significant differences (Pritts & Atwood,2002)
When using IM HCG the CPR, OPR & IR were significantly higher (Buvat et al,1990). The poor results obtained with oral P is related to its poor bioavailability.
No differences in CPR or IR (Farhi et al, 2000). The power of this study was low. 3. Vaginal Progesterone Vs P plus HCG: No differences in CPR or SAB (Ugur et al,2001).
III. Luteal phase support in ultrashort Protocol
In a single very small study, there were no significant differences in CPR or DR (Golan et al,1993). 2. Vag Progesterone VS P plus HCG: Vaginal P alone provides sufficient luteal phase support (Mochtar et al,1996).
Progesterone. 1. Vaginal P Vs placebo: No difference in PR (Polson et al,1992) 2. IM P Vs no treatment: PR was similar (Steirteghem et al,1988; Leeton et al,1985). P LPS is unlikely to have a significant effect on increasing PR.
2. Oral P, HCG or placebo: No differences (Kupfemrminc et al,1990). No necessity of P supplementation in the luteal phase if GnRH agonists were not used (Daya,1988).
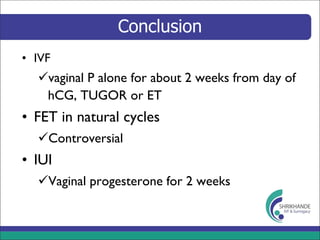
Vag P is more effective than oral P. Addition of oral E to P improves IR&PR in patients with profound E2 decline.
1. IM P with vag P; 2. different doses of P; 3. different forms of vag or IM P; 4. start of P at oocyte retrieval with start at ET.
Addition of ascorbic acid, prednisolone, aspirin to P has no benefit.
II. In direct protocol: No need of P supplementation in the luteal phase
Attitudes should shift towards milder stimulation protocols. This may reduce or eliminate the current Lacteal Phase defect.
Luteal phase support in ART - ppt video online download
Luteal phase support in ivf
Luteal phase support in IUI and ART, Dr. Laxmi Shrikhande, ShrikhandeIVF
Luteal phase support in IUI and ART, Dr. Laxmi Shrikhande, ShrikhandeIVF

PPT - Luteal phase support in ART PowerPoint Presentation, free download - ID:177865
Luteal phase support in IUI and ART, Dr. Laxmi Shrikhande, ShrikhandeIVF
Luteal phase support in ART

PPT - Luteal Phase Support in ART Cycles PowerPoint Presentation, free download - ID:3505347

Luteal phase support in art - revisited
Luteal Phase Support in ART Cycles - ppt video online download
Triggers and Luteal Support What, Why and How? - ppt video online download
Luteal Phase Support in ART Cycles - ppt video online download

Luteal phase support in ART